Numerical alterations in the number of leukocytes or white blood cells are frequent causes of consultation to the clinical hematologist. Leukopenia is called the decrease in the normal number of leukocytes and leukocytosis is its increase with respect to the values considered normal.
Leukopenia is a frequent consultation that worries the patient due to the possibility of suffering a greater susceptibility to infections. In this situation, the assessment of the number of neutrophilic granulocytes, that is, the type of leukocyte responsible for antibacterial defense, is essential. The vast majority of patients who consult for this reason have a somewhat decreased number of neutrophilic granulocytes or neutropenia, but enough so as not to suffer greater susceptibility to infections. The hematologist assesses the possible causes of leukopenia and neutropenia that, in general, are usually benign.
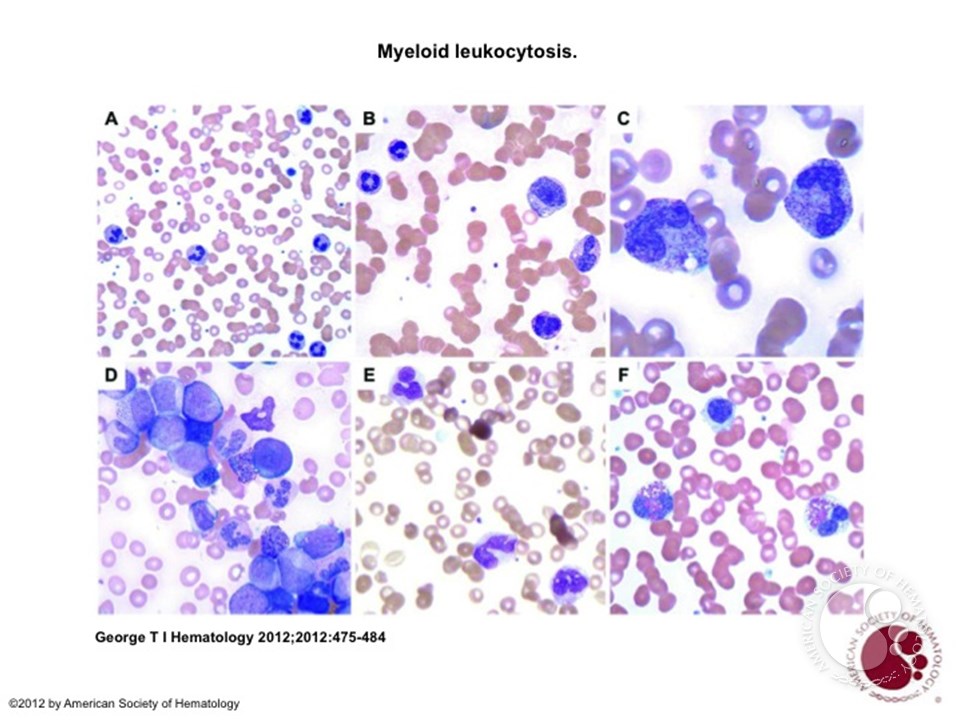
Leukocytosis can be the expression of an infection, pharmacological treatment with corticosteroids, smoking or a blood tumor disease, among other causes. In the first case, the increase is due to a reaction of the body against a bacterial infection, although, sometimes, a viral infection can produce the opposite effect or leukopenia.
Treatment with drugs or preparations containing corticosteroids can cause neutrophilic leukocytosis. In this case, identification of the drug provides the diagnosis. Smoking can cause leukocytosis with increased neutrophilic granulocytes (neutrophilic leukocytosis) in a variable number of smokers.
A relatively frequent consultation is the increase in the number of leukocytes at the expense of the number of lymphocytes, the cells responsible for defense against viral infections. Lymphocytosis or an increase in the total number of lymphocytes can be observed in the course of infections by viruses such as Epstein-Barr (the most common in infectious mononucleosis) or other viruses, although it may also be a finding indicative of a chronic disease of the blood.
A persistent increase in the white blood cell count may represent the first change indicative of leukemia. When this possibility is suspected, the hematologist assesses the existence of adenopathies (enlarged lymph nodes) or splenomegaly (enlarged spleen), the description of the appearance of the leukocytes in the microscopic review of the blood smear and the symptoms that the patient refers.
Based on this basic information, an analysis of the immunological characteristics of the leukocytes is requested and, frequently, a bone marrow examination, together with the analysis of various genetic mutations that, together with the rest of the results, allow establishing the diagnosis. In general, the majority of leukemias are of the chronic type, many of them without symptoms and that are diagnosed as a result of an analysis carried out for other health reasons (routine controls), as opposed to acute leukemias, which very frequently cause a significant deterioration in general condition.
It is important to explain to the patient that the diagnosis requires sequential examinations and analyses, and therefore takes time. It is essential to have a certain diagnosis that allows a safe diagnosis to be made in order to establish an adequate prognosis and treatment.